Essential Considerations for Selecting Surgical Orthopedic Equipment
The selection of orthopedic instruments plays a crucial role in determining surgical success and patient outcomes. Medical professionals must carefully evaluate various factors to ensure their chosen instruments meet the highest standards of quality, precision, and reliability. Understanding the key aspects of orthopedic instrument selection helps hospitals and surgical centers make informed decisions that benefit both practitioners and patients.
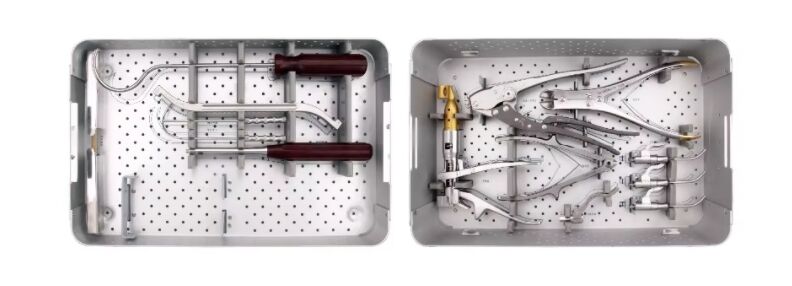
Modern orthopedic surgery demands instruments that combine innovative design with proven functionality. From basic hand tools to complex measurement devices, each piece must work seamlessly within the surgical workflow while maintaining strict medical standards. This comprehensive guide explores the critical factors in selecting orthopedic instruments and provides valuable insights for healthcare facilities seeking to optimize their surgical equipment inventory.
Material Quality and Manufacturing Standards
Superior Materials for Lasting Performance
High-grade stainless steel remains the gold standard for orthopedic instruments, offering exceptional durability and resistance to corrosion. Surgical-grade steel alloys, particularly those meeting ASTM F899 specifications, provide the optimal balance of strength and longevity. These materials ensure instruments maintain their precise dimensions and cutting edges through repeated use and sterilization cycles.
Advanced coating technologies, such as titanium nitride or diamond-like carbon, enhance surface properties and extend instrument life. These coatings reduce friction, improve wear resistance, and provide better visibility during procedures. When evaluating orthopedic instruments, checking material certificates and manufacturing documentation helps verify compliance with international standards.
Manufacturing Precision and Quality Control
State-of-the-art manufacturing processes ensure consistent quality across all orthopedic instruments. Computer-aided design and precision machining create tools with exact specifications and tight tolerances. Quality control measures, including dimensional verification and material testing, guarantee each instrument meets rigorous performance standards.
Regular inspection protocols and documentation of manufacturing processes provide traceability and confidence in instrument quality. Healthcare facilities should partner with manufacturers who maintain ISO 13485 certification and follow Good Manufacturing Practice (GMP) guidelines to ensure reliable, high-quality orthopedic instruments.
Ergonomic Design and Functionality
Optimized Handle Design and Weight Distribution
Ergonomic considerations significantly impact surgical performance and user comfort. Well-designed orthopedic instruments feature handles that provide secure grip and precise control while minimizing hand fatigue during lengthy procedures. The weight distribution must feel natural and balanced, allowing surgeons to maintain steady movements and accurate placement.
Textured surfaces and contoured grips enhance instrument handling in wet conditions, while thoughtful design elements reduce the risk of repetitive strain injuries. Evaluating these ergonomic features through hands-on testing helps ensure selected instruments meet the physical demands of orthopedic surgery.
Functional Versatility and Specialized Applications
Modern orthopedic instruments often serve multiple functions, streamlining surgical workflows and reducing inventory requirements. Modular systems and adaptable tools provide flexibility across different procedures while maintaining specialized capabilities for specific applications. Understanding the full range of instrument functionality helps optimize selection for diverse surgical needs.
Consider instruments that offer clear marking systems, intuitive adjustment mechanisms, and compatibility with existing surgical systems. This approach ensures efficient integration into current protocols while maintaining the highest standards of surgical precision.

Sterilization and Maintenance Requirements
Sterilization Compatibility and Processing
Orthopedic instruments must withstand repeated sterilization cycles without degradation. Materials and construction methods should be compatible with standard autoclave procedures and chemical sterilization methods. Instruments with complex mechanisms require special attention to ensure complete sterilization of all components.
Evaluate cleaning requirements and access points for proper maintenance. Instruments with smooth surfaces and minimal crevices facilitate thorough cleaning and reduce the risk of contamination. Documentation should clearly outline recommended sterilization parameters and maintenance procedures.
Long-term Durability and Maintenance Protocols
Establishing clear maintenance schedules and inspection criteria helps extend instrument life and maintain optimal performance. Regular assessment of cutting edges, joint function, and surface condition identifies potential issues before they impact surgical outcomes. Proper care and maintenance procedures should be easily integrated into existing facility protocols.
Consider the availability of maintenance services and replacement parts when selecting orthopedic instruments. Reliable manufacturer support and warranty coverage provide additional assurance of long-term value and performance reliability.
Cost Considerations and Value Assessment
Initial Investment and Long-term Economics
While premium orthopedic instruments often carry higher initial costs, their superior durability and performance typically deliver better long-term value. Calculate the total cost of ownership, including maintenance requirements, expected service life, and potential replacement needs. Quality instruments that maintain precision and reliability reduce the frequency of replacement and minimize disruption to surgical schedules.
Consider volume requirements and usage patterns when evaluating instrument investments. Bulk purchasing options and package deals may offer cost advantages while ensuring consistent quality across the instrument inventory.
Return on Investment Analysis
Evaluate the impact of instrument quality on surgical efficiency and outcomes. Higher-grade orthopedic instruments can reduce procedure times, improve precision, and enhance overall surgical performance. These benefits contribute to better patient outcomes and increased procedure volumes, supporting the business case for quality instrument investment.
Track performance metrics and maintenance costs to quantify the value of instrument selections. This data helps inform future purchasing decisions and optimize instrument inventory management.
Frequently Asked Questions
What certifications should I look for when purchasing orthopedic instruments?
Look for instruments that meet ISO 13485 standards and FDA requirements. Manufacturers should provide documentation of material certifications, quality control processes, and compliance with relevant medical device regulations. CE marking is essential for instruments used in European markets.
How often should orthopedic instruments be replaced?
The replacement frequency depends on usage patterns, maintenance practices, and visible wear. Generally, high-quality orthopedic instruments should last 5-10 years with proper care. Regular inspection and maintenance help identify when replacement is necessary to maintain optimal performance.
What are the most important factors in maintaining orthopedic instruments?
Proper cleaning, sterilization, and storage procedures are crucial for instrument longevity. Following manufacturer guidelines for care and maintenance, conducting regular inspections, and addressing wear issues promptly help preserve instrument quality and functionality. Staff training on proper handling and maintenance procedures is also essential.
 EN
EN
 FR
FR
 ES
ES
 AR
AR