Introduction to Premold Titanium Mesh in Craniofacial Surgery
The Evolution of Craniofacial Reconstruction
Craniofacial surgery has evolved from basic techniques to advanced procedures that improve patient outcomes. Initially, treatments were limited, relying heavily on reconstructive practices that offered minimal results and carried higher risks of complications. However, the advent of alloplastic materials in the 20th century marked a significant milestone. These materials paved the way for modern reconstruction techniques that focus on both aesthetic and functional rehabilitation. Significant advances have been made through collaboration between technology and materials science, leading to the production of engineered implants such as titanium mesh. Scientific studies indicate that these innovations have resulted in reduced complication rates and accelerated recovery times, enhancing the prospects for successful craniofacial surgery.
Role of Titanium Mesh in Modern Surgical Practice
Titanium mesh has become an integral component in contemporary craniofacial surgery, offering vital structural support and helping to restore anatomical accuracy. Its unique properties, like lightweight strength and resistance to corrosion, make it ideal for various surgical procedures. Clinical evidence indicates that utilizing titanium mesh enhances outcomes, thus establishing it as a transformative element in modern surgical practice. Recent studies document its efficacy and continue to explore its potential uses beyond simple reconstruction, underlining its adaptability and enduring importance in craniofacial operations. Consequently, titanium mesh is not merely a tool but a catalyst for future advancements in the field.
What Is Premold Titanium Mesh?
Material Composition and Biocompatibility
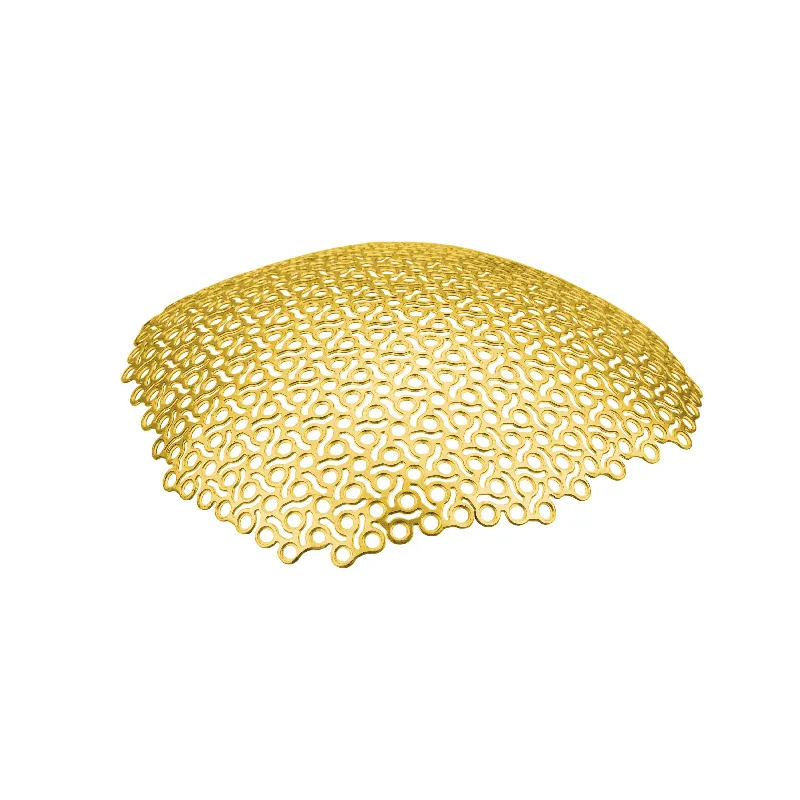
Premold titanium mesh is crafted from high-purity titanium, renowned for its exceptional biocompatibility and minimal rejection rates. The porous structure of the mesh allows for significant tissue ingrowth, which facilitates osseointegration, a crucial factor in successful surgical outcomes. Studies indicate that titanium is less prone to inciting inflammatory responses, making it a preferred choice in implantology, especially where biocompatibility is paramount.
Prefabricated Design and Manufacturing Process
The prefabricated design of premold titanium mesh enables surgeons to select pre-shaped implants that conform to specific anatomical requirements of patients. The use of cutting-edge CAD/CAM technology in manufacturing ensures high precision and uniformity in custom configurations of these implants. The advantage of such tailored solutions lies in reducing operative time and minimising the necessity for further modifications during or after surgery, enhancing efficiency and patient outcomes.
Historical Development in Surgical Applications
The use of titanium in surgery has a rich history dating back to the 1950s, reflected in its journey alongside the evolution of surgical techniques. Initially rooted in orthopedic applications, titanium's appealing properties have seen its use extend into craniofacial surgeries. Over the years, as surgical methods have advanced, there has been a conspicuous uptrend in relying on titanium-based implants. This shift underscores the material's enduring significance in craniofacial reconstruction, promising improvements in both functional and aesthetic outcomes.
Key Applications in Craniofacial Procedures
Skull Reconstruction After Traumatic Injuries
Premold titanium mesh plays a significant role in skull reconstruction, especially after traumatic injuries such as fractures. It excels in restoring structural integrity and reducing complications compared to traditional methods. According to clinical outcomes, its use in reconstruction has demonstrated a marked improvement in patient recovery, largely due to its flexibility which allows for creating personalized treatment plans. This adaptability is crucial in addressing the unique injury profiles of each patient, ensuring tailored solutions that enhance recovery and outcome success.
Congenital Defect Correction
For congenital defects like craniosynostosis, premold titanium mesh offers revolutionary advancements in corrective procedures. Surgeons can mold the mesh to precisely fit the patient's unique cranial anatomy, resulting in significantly improved outcomes. This tailored approach has been highlighted in research as having increased success rates for surgeries targeting congenital defects. The use of titanium mesh in these procedures underscores its value in providing customized treatment options that significantly boost surgical success and patient recovery.
Orbital and Maxillofacial Restoration
Titanium mesh is indispensable in orbital and maxillofacial restorations, prized for its balance of lightweight strength and resilience. Surgeries in these areas gain significantly from the material's properties, leading to enhanced recovery times and elevated patient satisfaction levels. Data supports that reconstructive procedures using titanium mesh in the orbital and maxillofacial regions often result in high success rates. The ability of the mesh to withstand these complex surgical challenges while maintaining its structural integrity plays a crucial role in the overall enhancement of patient outcomes.
Advantages Over Traditional Reconstruction Methods
Surgical Precision and Reduced Operating Time
Utilizing premold titanium mesh offers precise anatomical reconstruction, significantly reducing the need for extensive sutures and adjustments. Research indicates that surgeries incorporating titanium mesh often result in shortened operating times compared to traditional methods, enhancing efficiency. This increased efficiency is particularly advantageous as outpatient procedures become more prevalent, directly correlating with improved hospital turnover rates. In effect, hospitals can manage more cases with the same resources, fostering better patient care.
Superior Biocompatibility and Osseointegration
The biocompatibility of premold titanium mesh surpasses that of many traditional materials, leading to more relaxed post-operative monitoring conditions. Studies suggest that titanium's excellent osseointegration enhances implant stability within the craniofacial structure, contributing to the durability and effectiveness of reconstructive procedures. Patients using titanium mesh report fewer complications related to implant rejection and inflammatory responses, underscoring the material's reliability in clinical settings and ensuring patient safety and comfort.
Long-Term Stability and Cosmetic Outcomes
Premold titanium mesh provides long-term stability in reconstructive procedures, ensuring outcomes are maintained over time. Clinical studies consistently show high patient satisfaction with cosmetic results due to the mesh's minimal visibility post-surgery. These successful cosmetic enhancements contribute to patients experiencing an improved quality of life, marking advancements in surgical techniques. The consistent long-term stability achieved with titanium mesh plays a crucial role in the durability and aesthetic appeal of craniofacial surgeries.
Future Trends in Titanium Mesh Technology
3D-Printed Custom Implants
3D printing technology is poised to fundamentally transform the realm of implant fabrication, offering unprecedented customization through titanium mesh solutions tailored to individual patient anatomy. This advancement leverages sophisticated imaging techniques combined with 3D printing to achieve extraordinary surgical precision by minimizing errors and enhancing implant alignment. The increasing adoption of 3D printing techniques in surgeries is anticipated to lead to cost reductions and improved accessibility for a wider range of patients.
Bioactive Coatings for Enhanced Integration
The development of bioactive coatings for titanium mesh is a promising area of research, aimed at improving the integration of implants within craniofacial structures. These coatings are designed to enhance bonding with surrounding tissues, potentially reducing healing times and improving surgical outcomes. Emerging studies indicate that such innovations could lead to improved osseointegration and reduced complications in craniofacial surgeries, highlighting a bright future for these technologies.
Resorbable and Smart Material Innovations
Exploration into resorbable and smart materials holds the potential to revolutionize titanium mesh technology. The future may witness the advent of resorbable meshes that offer temporary structural support before harmlessly dissolving, thereby eliminating the need for follow-up removal surgeries. Furthermore, smart materials capable of adapting to physiological changes present immense potential for personalized surgical interventions. Continued research in this area is expected to unveil novel applications, signaling a significant evolution in surgical strategies and methods.
FAQ
What is premold titanium mesh used for in surgeries?
Premold titanium mesh is used in craniofacial surgeries for reconstructing skulls after traumatic injuries, correcting congenital defects like craniosynostosis, and for orbital and maxillofacial restoration.
Why is titanium a preferred material for surgical implants?
Titanium is favored due to its high biocompatibility, resistance to corrosion, and its ability to support tissue ingrowth and osseointegration, leading to reduced inflammatory responses and complications in surgeries.
How do 3D-printed custom implants benefit craniofacial surgeries?
3D-printed custom implants provide unprecedented customization that exactly matches a patient’s anatomy, enhancing surgical precision, reducing errors, and improving overall surgical outcomes.
 EN
EN
 FR
FR
 ES
ES
 AR
AR