Premold Titanium Mesh in Modern Trauma Surgery
What Makes Titanium Mesh Ideal for Traumatic Injuries?
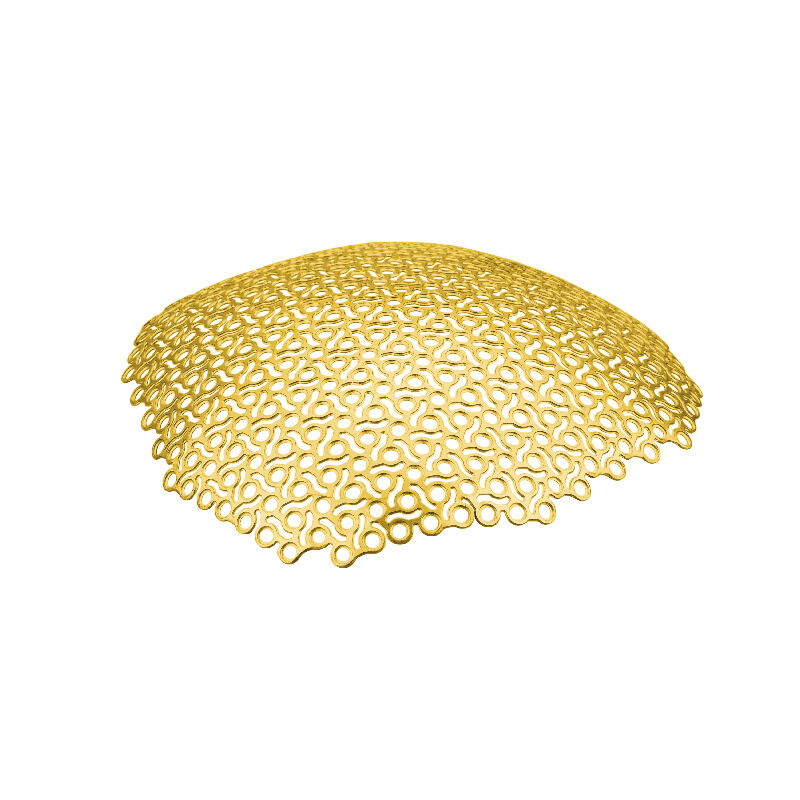
Titanium mesh is popularly considered for cases of traumatic defects because of its lighter weight and greater strength properties. It serves to hold broken bones in place securely and comfortably until they heal, while promoting mobility and proper healing. Because of the superior strength of titanium, bones remain in proper alignment during the healing processes. In addition, the corrosion resistance of titanium can contribute to prolonged wear, thus decreasing the probability of having complications due to the degradation of the implant. Excellent tensile strength of the mesh; the mesh is able to stand surgical manipulation of traumatic injuries, gives consistent support. According to orthopedic specialists, their research shows that the titanium mesh causes fewer failures than the materials previously used in surgeries, so it's "the best option" for modern day trauma care.
Evolution of Mesh Design in Orthopedic Repairs
Progress of mesh development in orthopedic repairThe development of meshes used in orthopedic repairs has represented an important transition from conventional materials to modern titanium, changing surgical approaches. With advances in titanium mesh design, developments are focused on supporting bone integration and research and development remain ongoing. These advancements involve surface texturing methods to enhance cell attachment and proliferation for faster tissue integration. Historical perspective has shown huge growth in titanium mesh over the past 20 years and its importance in trauma management. Mesh design technology is expected to evolve further in the future including bioactive properties, which also contribute to promote faster healing and improved patient prognosis and will strengthen the position of titanium mesh as a constituent technology of modern orthopedic surgeries.
Key Advantages of Premold Titanium Mesh Systems
Superior Strength-to-Weight Ratio for Structural Stability
Premold Titanium Mesh systems offer an excellent weight-to-strength ratio, which is an important parameter when it is used for maintaining bone architecture after surgery. This exclusive characteristic spares the surrounding tissues from excessive stress and pain, which promotes a much easier and quicker rehabilitation. Peer-reviewed reviews in orthopaedic literature show that titanium mesh provides superior stabilization compared with traditional, heavier materials, thus highlighting its advantages in challenging surgical settings. Its light weight also allows for ease of manipulation and implantation, making it valuable for operative procedures. In this issue, titanium mesh is some other treatment alternative this is associated with much less postoperative pain and faster rehabilitation, which is also supported by the available facts of patient restoration.
Biocompatibility: Minimizing Rejection Risks in Implants
The biocompatibility of titanium mesh systems considerably contributes to the risk minimization of implant rejection that is crucial for the success of these invasive procedures. It has been clinically confirmed that titanium induces a lower inflammatory response than other materials and the surgical efficacy and patient safety is also improved. Leading scientific bodies recommend the use of titanium as it can bond well with the human body, supported by long-term clinical testing of millions of patients. Existing research would further seem to indicate that post-implant complications/failures are significantly reduced in the case of titanium when compared to other, non-biocompatible alternatives. Both patient reviews and reputable studies agree on the necessity of using biocompatible materials for a safe and effective surgical outcome.
Pre-shaped Configurations for Rapid Surgical Implementation
As a result, prefabricated titanium meshes are ideally tailored to the surgical requirements, facilitating a fast and optimal implantation process. • The prefabricated forms of the grafts simplify surgery and save valuable time, an essential key to an optimal management and outcome of the patients. Contemporary surgical reports data suggests a significant reduction in complications associated with premolded systems due to its custom fit. As a result, surgeons report that pre-shaped implants provide increased satisfaction and a successful result, particularly in accommodating the variety of anatomical differences that they encounter. The future for preformed models appears to be bright, as we continue to evolve with new technologies that are bound to enhance the accuracy and effectiveness of surgery using the titanium mesh systems.
Common Trauma Applications in Clinical Practice
Cranial Reconstruction After Complex Fractures
Titanium mesh is the preferred cranioplasty material because of its superior strength and strength to weight ratio. When treating extensive cranial defects, surgical case series demonstrated improved cosmetic and functional results when using titanium mesh. Its efficacy is also affirmed by statistics, showing a high success rate in the reconstruction of cranial defects, and low incidence of complications. The exact fit of titanium mesh promotes the integrated aggregate with the host bone and heals completely after surgery. In addition, the development of minimally invasive procedures had made the use of titanium mesh in cranial repairs more acceptable, leading to a faster recovery and operation.
Facial Bone Repair in Polytrauma Cases
Cases with numerous facial fractures are well reconstructed using titanium mesh owing to its flexibility. The available clinical evidence indicates that titanium plating affords the best repositioning and stabilisation of multifragment complex facial fractures. This leads to a decrease in the recovery period in patients undergone titanium mesh implant than conventional method. In addition, facial asymmetry for example can be corrected by titanium mesh effectively and patient satisfaction can be increased greatly after operation. Advancements have been made in the recent years to tailor titaniun mesh to a patient's specific facial reconstruction needs to increase the accuracy and functionality of reparative procedures.
Rib and Sternum Stabilization Techniques
Titanium mesh can be used to stabilize fractures of the ribs and sternum, which is essential for lung healing and maximum pulmonary function. Studies have shown that stabilizing titanium mesh significantly reduces the risk of respiratory complications with rib injuries. The ease of intraoperative manipulation is commonly cited by the practitioners using titanium mesh systems. Comparisons have shown a lower incidence of postoperative complications in titanium mesh versus other types of fixation. Titanium mesh is recommended by surgeons due to its proven effectiveness and because of the successful results obtained in the treatment of thoracic trauma, making it an excellent option for such important applications.
Critical Surgical Considerations for Optimal Outcomes
MRI/CT Compatibility for Postoperative Monitoring
This is important to allow efficient post-operative monitoring of recovery, through clear imaging by both the MRI and CT scanners of the titanium mesh. Clinical protocols prefer titanium for its radiolucency, allowing for accurate diagnostics without implant related artifacts. Its been proven by statistical observation, imaging compatibility reduces reoperation for undetected complications. Continuous visualization of the healing process using precise imaging is a significant benefit of the use of titanium mesh. In addition, by precisely imaging the victims, research has found long term trauma care costs can be reduced by preemptively detecting and treating problems.
Intraoperative Flexibility: Reshaping and Securing Methods
Titanium mesh demonstrates great intraoperative moldability, as it can be modified and shaped to the particular anatomical condition of the individual patient. This versatility allows a surgeon to customized the shape and fit resulting in better patient results. Information from examinations during operations, suggests that the use of the flexible mesh, decreases complications in the operations. Recent technology makes operating room reshaping correlate with faster recovery and less postoperative pain for patients. “It’s innovative ‘normative’ if you think about it and say, ‘This applies to everybody,’” he says, adding that flexible solutions such as these are critical to achieve the best outcome in challenging trauma cases, offering patients a balance of function and aesthetics when it comes to reconstruction.
Future Directions in Titanium Mesh Technology
3D-Printed Patient-Specific Mesh Developments
With the recent availability of 3D printing technology, it has become possible that new individualized design of titanium mesh implants can be modelled directly by the operating surgeon on the patient's anatomy. Recent developments in this technology have minimized the production time and improved the mesh fit to an extend that has impacted positively on surgical results. Research reveals that these custom-fitted designs help improve the success of surgery manyfolds and contented feeling of the patients on account of individualization. The future direction of impromptu 3D printing in trauma surgery is slowly changing by providing customized solutions for challenging situations. Experts predict that additional advances in digital modeling and 3D printing technology are expected to continue to influence the future of health services for trauma care.
Surface Modification for Enhanced Osseointegration
Surface modifications of titanium mesh are important advancements to enhance osseointegration, which results in quick and reliable bone healing. Recent studies suggest that bioactive coatings remarkably enhance the results of implantation, where titanium based surgery materials are more successful. These surface coating methods have been promising to enhance the biocompatibility in the implants. Some statistics Modified titanium screws promote the dynamics of the cellular and vascular activity compared to the just untreated titaniumAnd that's progress people! In the future, the addition of advanced surface modifications will be a key development for further enhancing performance and life of TIM implants and to confirm their effectiveness when applied to a multitude of surgical procedures.
FAQ Section
What are the benefits of using titanium mesh in trauma surgery?
Titanium mesh is beneficial due to its lightweight nature, superior strength-to-weight ratio, corrosion resistance, and biocompatibility. These properties enhance structural stability, reduce implant rejection risks, and improve patient recovery.
How does titanium mesh compare to traditional materials?
Titanium mesh offers better stabilization and integration compared to traditional materials, displaying lower failure rates and fewer postoperative complications.
Can titanium mesh be used in facial reconstruction?
Yes, titanium mesh is highly adaptable for facial reconstruction, providing superior alignment and stabilization for complex facial bone injuries, addressing challenges like facial asymmetry.
Is titanium mesh compatible with imaging technologies like MRI and CT scans?
Yes, titanium mesh is compatible with MRI and CT scans, ensuring accurate postoperative monitoring without implant-related imaging artifacts.
How does 3D printing technology impact titanium mesh implants?
3D printing allows for creating patient-specific titanium mesh implants that improve precision, accelerate production, and enhance surgical outcomes through tailored treatments.
Table of Contents
- Premold Titanium Mesh in Modern Trauma Surgery
- Key Advantages of Premold Titanium Mesh Systems
- Common Trauma Applications in Clinical Practice
- Critical Surgical Considerations for Optimal Outcomes
- Future Directions in Titanium Mesh Technology
-
FAQ Section
- What are the benefits of using titanium mesh in trauma surgery?
- How does titanium mesh compare to traditional materials?
- Can titanium mesh be used in facial reconstruction?
- Is titanium mesh compatible with imaging technologies like MRI and CT scans?
- How does 3D printing technology impact titanium mesh implants?
 EN
EN
 FR
FR
 ES
ES
 AR
AR