Understanding Modern Approaches to Spine Surgery
Spinal surgery has evolved dramatically over the past decades, offering hope to millions suffering from debilitating back pain and injuries. Today's advanced surgical techniques provide precise solutions for various spinal conditions that haven't responded to conservative treatments. From minimally invasive procedures to complex reconstructive operations, spinal surgery represents a crucial intervention for patients seeking lasting relief from chronic back problems.
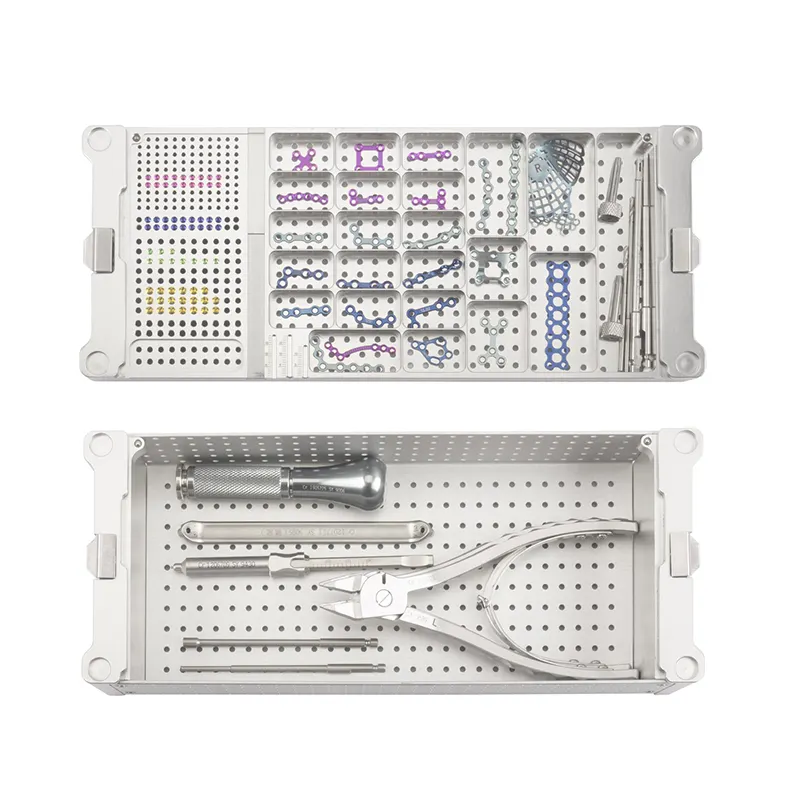
Modern surgical approaches focus not only on alleviating pain but also on preserving spinal function and promoting faster recovery. Surgeons now employ state-of-the-art imaging technology, computer-assisted navigation, and refined surgical instruments to achieve optimal outcomes. This advancement in surgical capabilities has transformed the landscape of spine care, making procedures safer and more effective than ever before.
Types of Spinal Surgical Procedures
Minimally Invasive Techniques
Minimally invasive spinal surgery represents a revolutionary approach to treating back problems. These procedures utilize small incisions and specialized instruments to access the spine, resulting in less tissue damage and faster healing. Surgeons can perform various operations through these tiny portals, including discectomies, decompressions, and even some fusion procedures.
The benefits of minimally invasive techniques extend beyond reduced scarring. Patients typically experience less post-operative pain, shorter hospital stays, and quicker returns to daily activities. Advanced imaging systems guide surgeons with unprecedented precision, ensuring optimal placement of hardware and minimal disruption to surrounding tissues.
Traditional Open Surgery Options
While minimally invasive techniques continue to gain popularity, traditional open spinal surgery remains essential for certain conditions. Complex spinal deformities, extensive tumors, or severe trauma may require the enhanced visibility and access that open procedures provide. These surgeries involve larger incisions but allow surgeons to address complicated issues that demand a more comprehensive approach.
Modern improvements in surgical techniques and equipment have enhanced the safety and effectiveness of open procedures. Surgeons now use sophisticated monitoring systems to protect neural structures and advanced implant materials that promote better fusion and long-term outcomes.

Conditions Requiring Surgical Intervention
Degenerative Disc Disease
When spinal discs deteriorate due to age or wear, they can cause persistent pain and limited mobility. Spinal surgery addresses severe cases through various techniques, including disc replacement or fusion procedures. These interventions aim to stabilize the affected segments and relieve pressure on compressed nerves.
Surgical treatment for degenerative disc disease often involves removing damaged disc material and either fusing the vertebrae or replacing the disc with an artificial implant. The choice between these options depends on factors such as the patient's age, overall health, and specific pathology.
Spinal Stenosis and Neural Compression
Spinal stenosis, characterized by narrowing of the spinal canal, frequently requires surgical intervention when conservative treatments fail. Decompressive procedures aim to create more space for neural elements, relieving pressure on the spinal cord or nerve roots. These surgeries can significantly improve mobility and reduce pain in affected patients.
Advanced surgical techniques allow for targeted decompression while maintaining spinal stability. In some cases, fusion may be necessary to prevent future complications or address concurrent instability issues.
Recovery and Rehabilitation Process
Immediate Post-Operative Care
The journey to recovery begins immediately after spinal surgery. Medical teams closely monitor patients' neurological status, pain levels, and vital signs during the initial recovery period. Early mobilization, when appropriate, helps prevent complications and promotes healing. Physical therapists work with patients to ensure safe movement and proper body mechanics.
Pain management strategies typically involve a multimodal approach, combining medications with careful activity progression. Modern protocols emphasize reducing opioid dependence while effectively managing post-operative discomfort.
Long-term Rehabilitation Strategies
Successful outcomes from spinal surgery depend heavily on comprehensive rehabilitation programs. Physical therapy focuses on strengthening core muscles, improving flexibility, and establishing proper movement patterns. Occupational therapy helps patients safely return to daily activities and work responsibilities.
Long-term success requires patient commitment to prescribed exercise routines and lifestyle modifications. Regular follow-up appointments allow surgeons to monitor healing progress and address any concerns promptly.
Technological Advances in Spinal Surgery
Robotic Assistance and Navigation
Robotic systems have revolutionized spinal surgery by enhancing precision and consistency. These platforms provide real-time imaging guidance and assist in optimal placement of surgical implements. The integration of artificial intelligence continues to improve surgical planning and execution.
Navigation technology allows surgeons to visualize complex anatomy in three dimensions during procedures. This enhanced visualization leads to more accurate hardware placement and reduced radiation exposure for both patients and surgical teams.
Biological Advances and Materials
Innovation in biological materials has expanded treatment options for spinal conditions. New generations of synthetic and biological implants promote better integration with natural tissue. Growth factors and stem cell applications show promise in enhancing healing and fusion rates.
Advanced materials used in spinal surgery combine durability with biocompatibility, improving long-term outcomes. Ongoing research continues to develop novel solutions for complex spinal pathologies.
Frequently Asked Questions
What determines if someone is a good candidate for spinal surgery?
Candidacy for spinal surgery depends on multiple factors, including the specific diagnosis, severity of symptoms, response to conservative treatments, overall health status, and imaging findings. Surgeons carefully evaluate these elements along with the patient's goals and lifestyle requirements before recommending surgical intervention.
How long is the typical recovery period after spinal surgery?
Recovery duration varies significantly based on the type of procedure and individual factors. Minimally invasive procedures may allow return to light activities within weeks, while complex reconstructive surgeries might require several months of rehabilitation. Your surgeon will provide specific timeline expectations based on your particular case.
What are the potential risks and complications of spinal surgery?
While modern spinal surgery is generally safe, potential risks include infection, bleeding, nerve injury, hardware failure, and adjacent segment disease. Surgeons discuss these risks thoroughly during pre-operative consultations and implement numerous strategies to minimize complications.
 EN
EN
 FR
FR
 ES
ES
 AR
AR